Key Takeaways
- Vasectomy is a reliable and straightforward method of permanent male contraception, supported by medical studies and increasing worldwide use.
- Understanding each stage of the vasectomy process helps individuals and couples make confident, informed choices about their reproductive future.
- Recovery is faster and easier than many anticipate, with most men returning to their routine within days.
- Personal circumstances, relationship status, and long-term goals all play a vital role in decision-making.
- Government and expert resources, like the CDC’s contraception guide, provide in-depth information about all available birth control options.
- There is a significant rise in the social acceptability of vasectomy, spurred by shifting gender roles and evolving conversations about family planning.
- Current reporting, such as the New York Times’ coverage of vasectomy trends, helps contextualize men’s experiences and societal shifts regarding this procedure.
What Is a Vasectomy?
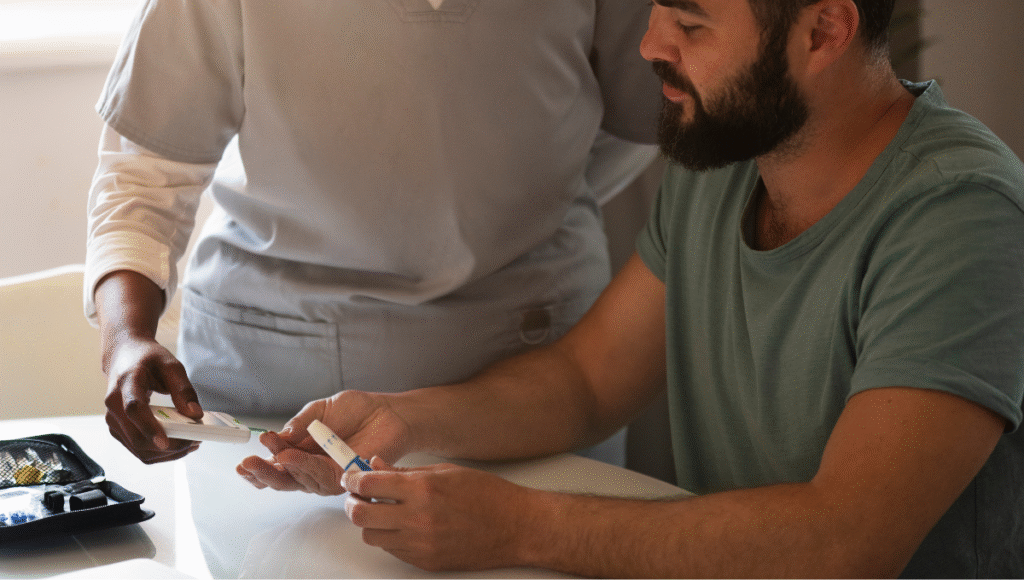
A vasectomy is often misunderstood, but at its core, it’s a reliable, straightforward surgical procedure intended to permanently prevent sperm from being released during ejaculation. During the process, a physician will cut and seal the vas deferens—the tubes that transport sperm—ensuring that sperm never reaches the semen. When speaking with a vasectomy doctor, individuals are often surprised by how minimally invasive the modern approach can be. This reassurance is rooted in decades of positive outcomes and continued medical refinement.The operation is relatively quick and almost always performed under local anesthesia in a doctor’s office or outpatient clinic. Most men spend less than 30 minutes undergoing the procedure. Techniques like the no-scalpel vasectomy further minimize discomfort, bleeding, and visible scarring. While permanence may seem daunting, practical counseling and transparent information allow prospective patients to weigh the benefits and feel secure in their choice. Medical studies confirm that vasectomy does not interfere with testosterone production, sexual arousal, or climax, which means the only thing that changes is the ability to father children.
Why More People Are Considering Permanent Birth Control
There has been a noticeable trend toward permanent birth control as family sizes shrink and the desire for long-term planning increases. Many couples appreciate the option of vasectomy as it provides peace of mind and relieves the ongoing responsibility often placed solely on one partner. Data from the Centers for Disease Control and Prevention (CDC) indicates that vasectomy is among the most effective contraceptive options, with a long-term failure rate of below 1%.This growing popularity can also be traced to cultural factors. As gender roles shift and more men take an active role in family health conversations, the vasectomy is seen not just as a medical procedure but as a proactive step toward shared family responsibilities. The feasibility of a short, outpatient procedure—coupled with the long-term benefit of eliminating the risk of unplanned pregnancies—gives many families a new sense of control over their future.
Common Questions and Concerns
- Does a vasectomy hurt? Fear of pain is a primary concern, but most report only mild discomfort or a tugging sensation during the procedure. Mild swelling or bruising is routine but resolves within a few days, rarely requiring more than ice packs and over-the-counter pain relief.
- How long does recovery take? The recovery period is brief. Many men return to work within two to three days, assuming their job is not physically strenuous. High-impact activities, heavy lifting, or sexual activity should be avoided for about a week to ensure proper healing and reduce the risk of rare post-surgical complications.
- Is a vasectomy reversible? This is meant to be a permanent method. Reversal techniques exist but are expensive, not always covered by insurance, and have variable success rates, especially as time passes since the original procedure. It’s essential for patients to feel confident about their decision.
- Does it affect testosterone or sexual function? Expert consensus confirms that vasectomy does not affect hormone levels or sexual performance. Sex drive, sensation, and the ability to achieve orgasm all remain unchanged. Some men even report reduced anxiety about unintended pregnancy, which can enhance intimacy and quality of life.
Potential Benefits
The advantages of vasectomy make it stand out from other permanent and temporary birth control options. From a cost perspective, a one-time procedure is much less expensive over a lifetime than continued use of pills, patches, or barrier methods. There’s also the convenience: no additional maintenance or doctor’s visits are required once healed. Unlike hormonal methods, vasectomy doesn’t introduce new chemicals into the body, nor does it require monitoring for side effects or interactions.
- Cost savings accumulate quickly, considering the expense of other contraceptive methods over the years or decades.
- The procedure is outpatient, often less than half an hour, and uses local anesthesia for comfort.
- There are no ongoing supplies, prescriptions, or refills necessary.
- It preserves natural hormone cycles and leaves sexual performance untouched.
- Long-term peace of mind is a recurring theme reported by couples after vasectomy.
Research repeatedly demonstrates that, compared to female sterilization—which involves abdominal surgery and higher risk—vasectomy is less invasive, has a much faster recovery time, and is almost always less expensive.
A Balanced View: Risks and Considerations
Every medical procedure involves some risk, though vasectomy is among the safest outpatient reproductive surgeries. The most common minor complications are bruising, swelling, or a dull ache. Infection risk is extremely low when aftercare instructions are correctly followed. For some, psychological adjustment plays a role; regret rates are low but not nonexistent, especially for those who make hasty decisions or encounter unexpected life changes down the road.Social and emotional considerations are as important as physical ones. Before scheduling a surgery, open, honest communication with a partner and a thorough discussion with a doctor are strongly advised. Making an informed choice reduces the risk of regret and allows for support from loved ones throughout recovery. To explore society’s shifting view and the context in which more men are choosing vasectomy, check the New York Times analysis on vasectomy trends for real-world perspectives and the stories behind the data.
Preparing for the Procedure
Good preparation leads to smoother recovery and peace of mind. Preparation includes clarifying goals, discussing motivations with your partner, and consulting a trusted healthcare provider. To minimize risks, Doctors typically review your medical history, allergies, and previous surgeries. Patients are often told to avoid blood-thinners for several days beforehand and to arrange for someone to drive them home.
Checklist for Preparation
- Have an open, judgment-free conversation with your partner about family plans and expectations.
- Finalize and disclose your health history with your doctor to tailor the procedure safely.
- Whether small or personal, write down concerns or questions to discuss before surgery day.
- Set up a comfortable recovery space at home and arrange time off work and social obligations following the procedure.
Small steps, like having comfortable ice packs and loose clothing ready, can make a big difference in recovery comfort.
Alternatives to Vasectomy
For individuals or couples not fully committed to making a permanent decision, there are many other contraceptive options. Condoms continue to be a popular, non-permanent choice, while hormonal methods like birth control pills, injections, or implants serve those preferring time-limited options with high rates of effectiveness. Intrauterine devices (IUDs) provide an alternative with durability but allow removal if family plans change.The best route is to evaluate long- and short-term goals, assess comfort with reversibility, and weigh each method’s side effect profile. Seeking guidance from a healthcare provider ensures alignment between method, health status, and life stage, allowing optimal satisfaction and minimal stress about future choices.
Life After Vasectomy: What to Expect
After a short recovery—typically a few days of rest and avoidance of heavy activity—most men resume work and everyday routines with no lingering issues. The most noticeable change is a lasting sense of reassurance about birth control. Post-procedure, doctors recommend at least one semen analysis to confirm success, as sperm may linger for up to a few months in the reproductive tract.After sharing the decision, many men and their partners express a new sense of partnership and trust. Honest discussion remains important: be alert to any unusual pain or swelling, and always follow up with your doctor as directed. For continued learning or to explore other contraception choices down the road, the CDC’s comprehensive resource on birth control is a great starting point.As society and family goals evolve, so do the reasons for choosing a vasectomy. What remains constant is the importance of making well-informed decisions with knowledgeable support, ensuring that any step taken is genuinely right for each individual and their loved ones.